Former Powerhouse Operator Ready To Leap Next Hurdle
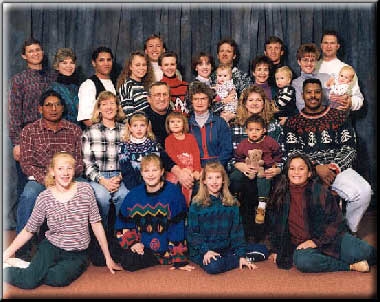
Ray and June Wadas were high school sweethearts at St. Paul High School in St. Paul, Nebraska. They were married in 1953, a few months after their graduation from high school. June bore Ray five sons and two daughters, all now adults, ranging in age from 46 to 33 years old. As you can see, the Wadases' children bore children of their own, and family get-togethers are big occasions.
"Valley Fever" Prompts Visit to Pulmonary Doctor
Before falling ill, Ray was very healthy, strong, and in great shape for his age. In mid-May, Ray became short of breath on a short vacation to Phoenix. At first, he thought that he had "valley fever", as it was windy and dusty in Phoenix. He consulted with his personal physician upon his return to Johnstown. On May 23, he met with his doctor again, and scheduled another appointment for June 2. Ray's symptoms became severe, and he was hospitalized on May 31. Chest films showed a fluid build-up on the left side. A CT scan and flexible tube bronchoscopy were non-diagnostic.
A pulmonologist performed a left-sided thoracentesis at North Colorado Hospital in Greeley, Colorado, removing approximately two liters of fluid from the chest cavity. On June 14, a thoracic surgeon performed a repeat thoracentesis, removing another two liters of fluid, as well as a thoracotomy with biopsy and talc insufflation at North Colorado. The pathology department returned the diagnosis of malignant mesothelioma the next day.
Local Doctors Baffled
The Wadases are a close-knit family. The Wadases' children began scouring the Internet for answers to the frightening enigma of mesothelioma. The Wadases learned what questions to ask. Typically, their local doctors could not provide answers. Even after a referral to a Greeley oncologist, there was no answer to whether the cell type was epithelioid (slow moving), or the more aggressive sarcomatous or bi-phasic types. There was no answer to the question of what stage Ray's mesothelioma had reached.
The tumor continued to rage within Ray. Night sweats left his t-shirts and bedsheets drenched. One night, June had to change the sheets five times. Despite a good appetite, Ray lost thirteen pounds from his gridiron frame of five feet eleven inches, 220 pounds.
Ray Considers Lovastatin
The first step Ray took was to go on Lovastatin, which he had heard would not only control his cholesterol but also restrict the blood flow to the mesothelioma tumors. In 1998, Dr. Jeffrey Rubin at the University of Minnesota demonstrated in laboratory mice with induced mesothelioma that this cholesterol lowering drug had anti-tumor potential, but there have been no reported translational studies with humans. Like William Dunn, Ray takes the Mevacor brand and reports no ill side effects.
Dr. Pass Promptly Returns Phone Call
The next thing Ray did was set up an appointment with the doctors at the University of Colorado in nearby Denver for July 5. With an assist from this website, Ray also phoned Dr. Harvey Pass, Chairman of the Science Advisory Board of the Mesothelioma Applied Research Foundation (MARF), a not-for-profit corporation which aims to eradicate mesothelioma as a life-ending disease. Dr. Pass returned his call the same day. They scheduled an appointment for Monday, July 17 at Harper Hospital in Detroit, Michigan.
Before meeting with Dr. Pass, Ray testified at a deposition which was expedited so that his evidence would be preserved for trial, and he could focus all of his energy on getting well. Ray detailed massive exposures to asbestos over the course of a 33 year career at powerhouses and a nuclear power plant operated by the Public Service Company of Colorado.
Dr. Pass Recommends EPP Without Delay
After flying to Detroit on Saturday, July 15, and setting up in Harper Hospital Guest Housing, the Wadases met with Dr. Pass' staff the following Monday for tests, including an MRI and chest films. On Tuesday, July 18, the Wadases met with Dr. Pass for the first time. After review of the test results and Ray's medical history, Dr. Pass recommended extrapleural pneumonectomy (EPP) surgery, consisting of removal of the left lung, part of the diaphragm, part of the pericardium (the lining around the heart), the pleura (the lining around the lung), and a rib. Dr. Pass would also resection the ribs on the left side during the surgery.
Ray asked whether trying a cycle of chemotherapy using ALIMTA (R) (pemetrexed disodium) or Gemcytabine and platinum would make sense. Dr. Pass replied that chemotherapy would weaken the immune system and diminish the likelihood of a successful surgery. Ray decided to go ahead with the EPP.
Dr. Pass, with characteristic dispatch, scheduled the surgery for 10:30 am the next morning!
Ray reported to pre-op two hours before surgery. Nurses inserted the epidural catheter used to control the pain. Surgery commenced promptly at 10:30 a.m. Every hour on the hour, Dr. Pass had an assistant call the Wadas family members gathered in the recovery room with updates. Dr. Pass had predicted that the surgery would take five hours. Sure enough, Dr. Pass emerged from the operating room five hours after beginning to report that the surgery had gone extremely well. He felt it was one of the "cleanest" EPPs he had ever done, in the sense that he felt there was a clean separation from the tumor he had removed and the (apparently) disease-free tissue remaining after surgery.
ICU Nurses take "Special Care" of Ray
Ray was taken to the recovery room at 3:30 p.m.. He had tubes going in and out of him in every direction, but he could talk okay. He remained in the recovery room for seven hours, because no space was yet available in the Intensive Care Unit (ICU). He was awake and feeling some pain, but he talked with his family and joked around with the nurses. Ray's family gathered about him when he arrived in ICU, and Matt, whom Rod calls "an impressive ICU nurse", assured them he would take special care of Ray that night.
On Thursday, July 20, the first day post-op, Ray was in good spirits, although in some pain. The nursing staff tried to get him to sit in a chair earlier in the morning, but were unsuccessful because his blood pressure was too low. Ray nearly passed out from the pain and the low blood pressure. He was a couple of pints short of blood, and the nurses gave him a transfusion.
Kim, an ICU nurse for 23 years, finally got Ray in a chair. At this point, his stomach was distended to the size of a watermelon. Apparently, stomach gases and air in his chest from the surgery were causing a pressure imbalance. Dr. Pass said he would use a long needle to relieve the pressure. The epidural was removed that evening.
Stomach Pressure and Pain
On Friday, July 21, Dr. Pass put a tube back through Ray's nose and down his throat to relieve the pressure on his stomach. Ray had vomited during the night, and the pain was excruciating.
On the Saturday morning of July 22, Ray's medical team felt he was out of the woods. Unfortunately, Ray had an apparently poor reaction to a pain medication which he had switched to. For a couple of hours, Ray recalled that he felt like he "was near death." He started to slip into a coma-like state where his respiration almost ceased. Ray's room in ICU was packed with doctors and staff. With their help, Ray pulled through, but his heart was beating very fast -- at 140 beats per minute.
Over the next few days, Ray Wadas slowly recovered. A day after his brush with death, he sat in a chair twice. He continued to experience a lot of pain in his throat from the tube running from his nose to his stomach. Pneumonia is always a concern with an EPP, and Ray had to sit up and cough to avoid pneumonia setting in.
By Monday, July 24, Ray was finally out of ICU. Dr. Pass felt if he continued his progress, he would be able to leave the hospital the following Saturday. They discussed the critical issue of how to handle post-operative care once Ray returned home. (Some local hospitals and doctors do not possess the know-how to render proper follow-up care post- EPP). Ray ate some Jell-O, the first substance approaching solid food he'd had since the preceding Tuesday.
By Tuesday, July 25, Ray had been removed from the morphine drip, and was in quite a bit of pain. The level of care dropped once he got out of ICU, which was frustrating to the Wadases, but this may have represented a little tough love treatment. Regardless, Ray was very motivated to get out of the hospital as quickly as he could!
Ray Walks out of Hospital, Hopeful
By Thursday, the Wadases were informed that Ray would be released from Harper Hospital Friday afternoon to Guest Housing, and then fly back to Denver the following day. Ray started feeling better after the pain pills given in lieu of the morphine drip took effect. His pulse rate continued to drop to more normal levels. Ray was in good spirits, eating well and moving well. He walked up and down the hospital halls with a walker. Ray said, "I could have walked a little faster, if I had only remembered to bring my tennis shoes!"
The same day, Dr. Pass gave the Wadases the report from the biopsy of his chest nodes. Of the thirteen nodes, eleven were negative and two positive. Dr. Pass also said that Ray has the "biphasic" form of the disease, which means it is a mix of epithelioid and sarcomatous tumors. The plan on discharge is for Ray to begin chemotherapy with Gemcytabine and Cisplatin in Denver as soon as he starts feeling well -- probably in four weeks.

Revered Pop Warner Football Coach
From the time word got out in Johnstown of Ray's diagnosis, the phone calls poured in from dozens of friends and family wishing him well. Ray is a respected and loved community leader. "Coach Wadas" helped found the Little League in Johnstown. He coached all of his sons, and of course others, for fourteen years. He coached Pop Warner football. He served on the Johnstown Town Board, and was "drafted" to serve one term as Mayor from 1989 to 1993. When he came to Johnstown thirty years ago, there was no Catholic church there. He helped make St. John the Baptist Catholic Church in Johnstown a reality. He has served as the Parish Council President. He and June ran a restaurant, a hardware store and a car wash.
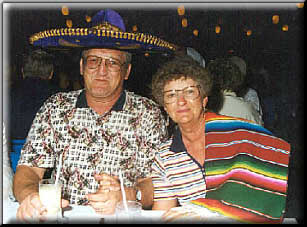
Ray and June finally retired a year ago. A self-described "golf addict" and travel lover, he and June have seen Paris, France, and traveled extensively in Denmark, where June has relatives. They have been to England and Germany, and taken an Alaskan and a Caribbean cruise. Every year, the children and grandchildren create a "romantic" dinner evening for Ray and June. The Wadases know how to have fun -- as this photo from Mexico amply demonstrates!
A Quiet Patience Unfettered by the Grim Odds
Ray and June can look back on a bright constellation of happy memories. Every day, they can greet someone whose life Ray has touched and bettered through parenting, coaching, or civic service. As Ray contemplates the future, he knows the odds are against him, but he doesn't think about the odds. He brings patience, the kind of quiet patience that can sit through tedious Town Board meetings and help neighbors at odds compromise for the common good. He brings discipline and respect for the rules of the game, traits he instilled in his children and others. He draws on the strength of a family he made strong, and on his faith in God.
Ray Wadas is one of us. When we pray for him, we pray for the best in us. Our thoughts and prayers are with the Wadas family as they tackle mesothelioma head-on.
*** POSTED AUGUST 21, 2000 ***
An Update on Ray from his son, Rod Wadas - 12/19/00
I just got back from Denver International. Ray and June are en route to San Antonio! They asked me to send you and your office, especially Trey Smith their sincere appreciation for all that you have done. You are a Godsend! Without any hyperbole, let me say that you have made a huge difference--we have hope where we had none.
Dr. Kelly sent their medical records to San Antonio last week. Ray and June scheduled an appointment for Thursday morning, December 21, at 9:00 for an evaluation. They are going there hoping to get into an Phase 1 ALIMTA trial, but it sounds like other trials might also be available. One of the most interesting aspects is a voluntary tumor "assay" which uses his tumor cells in a laboratory test with different chemotherapy treatments. Results are returned in 14 days. Based on results from 2600 tests, researchers have found that if the tissues from the biopsy react to the chemotherapy agent in the lab, there is a 78 percent likelihood that it will do so in the body. Just as importantly, if the tissues do not react to the chemotherapy agent in the lab, there is a 98% chance that the treatment will be ineffective in the body. That is stunning! There is nothing worse than the thought of going through ineffective, painful, useless chemotherapy. If we can be assured that the chemo works in the lab, that is the most powerful recommendation available. Seeing them leave for San Antonio is a wonderful Christmas gift. Thank you Trey! Everyone in my family thanks you!
My dad is getting a little weaker but he is as determined as ever to fight mesothelioma. Thanks to your help, he has found a way to keep fighting.
Regards, Rod Wadas
*** POSTED DECEMBER 21, 2000 ***
Mr. Wadas passed away on July 17, 2001