Anatomy of an Extrapleural Pneumonectomy
Six months ago, Sam Paffile began to experience fatigue and dark red blotches on his skin. Then on a recent trip to Mexico, Sam developed severe pains on the right side of his chest and was diagnosed with tuberculous pleuritis ( an inflammation of the pleura as the result of tuberculosis). He was immediately placed on antituberculous medications. Upon his return, he sought confirmation of the illness. It was not tuberculosis!
A thoracentesis (a surgical puncture of the chest for removal of fluids) and a pleural biopsy was performed on June 21, 1997 by Dr. Allen Muramoto at the Swedish Medical Center in Seattle, Washington. A diagnosis of epithelial mesothelioma was confirmed by both Swedish Medical Center and Dr. Samuel Hammar of Diagnostic Specialities Laboratory, Inc. in Bremerton, Washington. Dr. Hammar is a member of the elite U.S.-Canadian Mesothelioma Panel.
Dr. Ralph Aye, a pulmonary surgeon at Swedish Medical Center, discussed the possibility of a radical extrapleural pneumonectomy with Sam and his family. The risks are great. According to Dr. Aye there is a 5% to 8% mortality risk, and the results in the past have not always been what they had hoped. However, for Sam it seemed the best approach.
Preparations were made. Dr. Aye and his staff collaborated with Dr. Valeri Rusch at Sloan Kettering in New York regarding the tri-modal therapy. This protocol consists of removing the pleural space (pleurectomy), intrapleural infusion of chemotherapy and intense radiation. Sam, took all the steps necessary to prepare for his surgery. He had always taken care of himself, a robust man that looked younger than his 58 years of age. He did not smoke. On July 7, 1997 Sam Paffile was admitted to Swedish Medical Center for surgery.
Sam was wheeled into surgery at approximately 3:30 p.m. where a general anesthetic was administered. A double lumen endotracheal tube (a tube used inside the trachea to provide an airway through the trachea) was inserted and cuffed (inflated); along with all the other numerous tubes necessary to monitor the vitals of Sam. He was place on his left side, his chest shaved, prepped and draped in the usual sterile fashion.
A standard posterolateral thoracotomy incision (back to front) was made over the sixth (6th) rib from the scapula (right shoulder blade) to the spine. The muscle layers were divided and a rib spreader was put in place. The pleura (membrane around the lung and diaphragm) was peeled off and a large section of the diaphragm was removed. When they dissected the pleura off of the tissue (mestiastiumun) around the heart they found that the tumor had spread and that it was necessary to remove all of the mass tissue and a portion of the right side of the pericardium (sac) surrounding the heart. The heart, its large vessels, the trachea, esophagus, thymus and lymph nodes were all found intact and healthy. Also preserved were the azygos vein, superior vena cava, inferior vena cava and the internal mammary artery. Any bleeding from the intercostal vessels was controlled with clips or 3-0 silk ties.
The next step was to remove the right lung. There was some difficulty removing the root (pulmonary hilum) of the lung. First, the right mainstem bronchus was dissected out, and a heavy wire stapler was used to divide this. The pulmonary artery, inferior and superior pulmonary veins were all dissected out and stapled. Once all the attached vessels were removed the right lung, including the parietal pleura was removed and sent off to pathology. Two ribs, the third and eighth, and portions of three other ribs were also removed.
It was then time to put Sam back together again. Remember we told you that Sam had the top half of his diaphragm removed. This was replaced by using a 10 x12 cm piece of Gore-Tex sutured to the remaining diaphragm with 2-0 Prolene suture in a running stitch. Another piece of Gore-Tex, 8 x 12 cm, was used to repair the pericardial defect (the sac around the heart). There was a leak found on the thoracic duct, which was repaired. Before the closure of the chest a 28 French chest tube was inserted into the inferior portion of the chest. The ribs were mended using a #1 PDS suture. All of the layers of muscles were then closed using a #0 Vicryl running stitch. The shoulder blade was closed and the skin was sutured in place using a running 3-0 Vicryl subcuticular stitch. (This is a buried horizontal stitch in which the needle is passed under the skin through the edge of the wound and back again).
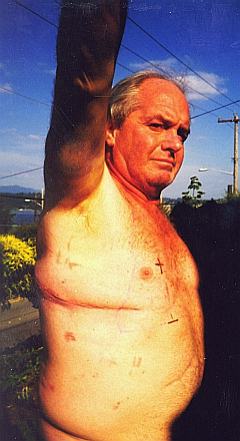
The operation lasted almost eight hours. Sam was back in the recovery room at 11:53 p.m. The following day, July 8, 1997, chest x-rays were take. It showed that fluid was beginning to fill the empty thoracic cavity. The catheter and the tube positions were secure and the heart size was stable. The portable chest x-rays over the next few days, through July 11, 1997, appeared to be consistent with the x-ray of July 8, 1997. On July 10, Sam was moved out of intensive care to the floor. He continued to be monitored, having his pain medication adjusted and on July 11, 1997 the epidural catheter was removed. On the morning of July 12, 1997 Sam was discharged from the hospital, and sent home.
Later that afternoon however, Sam was returned to the hospital and was seen in the emergency department. Sam had gotten his arm stuck in the bed railing the night before and on the way home the door was slammed on him, causing him further discomfort. Also, there was increased swelling above and below his incision and he was having trouble breathing. He told the attending doctor that there was a strange tightness or heaviness on his diaphragm and that he was having trouble moving. Mr. Paffile was re-admitted to the hospital for observation. His pain medication was adjusted and his incision was iced to decrease the swelling. He was discharged the following morning.
Sam went home for a few days. Around July 17th he began to have trouble breathing during the night. He found that he would have to sit upright to sleep and there was an increased pain on his right side when he tried to move his right arm. On July 19, 1997 he was brought to the emergency department at Swedish Medical Center by his wife, Marlene. Upon examination he was immediately placed on a cardiac monitor which showed an abnormal heart rate between 170 - 200. (Anything over 100 beats per minute is considered abnormal). An IV was established and oxygen was administered. Once the IV's were in place he was given six (6) milligrams of Adenocard IV, however there was no change. Another twelve (12) milligrams of Adenocard was given, and Sam suffered a sudden shortness of breath. The monitor slowed to a rate of 40 beats per minute, but shot up again to 180. Sam was in trouble. The attending physician, Dr. Rita Mellema, opted to administer Lidocaine. Approximately, three minutes after the Lidocaine was administered, Sam's chest pain ceased and normal sinus rhythm began, easing his breathing difficulties.
Sam's remaining time in the emergency department was satisfactory. He continued to have a normal sinus rhythm of 80 - 90, and he had no recurrent episodes of breathing problems or chest pain. Of course, Sam was admitted to the hospital for close observation and monitoring. He was examined thoroughly by doctors and released the following day.
Since that time, Sam has been doing well. On July 29, 1997, he was admitted to Swedish Medical Center under the care of Dr. Gary E. Goodman to begin his chemotherapy and radiation. Sam is scheduled to have radiation treatments every day for five weeks. After that time, Sam will be evaluated.
** POSTED AUGUST 21, 1997 **
Mr. Paffile passed away on June 25, 1998

